What to Know
- Researchers at Penn Medicine are hoping to understand what CDKL5 is and if cannabis can help patients diagnosed with the disorder.
- Harper Howard was born with a fatal and rare genetic disorder called CDKL5.
- Little is known about the condition, other than it causes violent seizures and cannot be cured.
Penny Howard arrived in Philadelphia last month anxious to see her daughter, Harper, again. It had been more than one year since Penny's little girl died from a rare disease called CDKL5 that marked her short life with violent seizures and developmental disorders.
Her daughter now lives on through groundbreaking research being done at Penn Medicine that could eventually help others with the disorder. Doctors and researchers there are trying to understand what caused her seizures and what could have been done to treat them. Among those possible remedies is cannabis. Howard believes Harper proved it before dying last year.
“Oh wow!” Howard said while gazing at a tiny sample of her daughter’s brain. It was dyed a bright pink and would soon be magnified under a microscope.
Taking a minute for herself, the Texas mom reflected on what it means to see her daughter in this way.
“We really walked a fine line of hope and hopelessness for a very long time. Because we realized that this was something bigger than what we were able to fix,” she said.
Harper Howard was just two weeks old when she had her first seizure. By 19 months, she was having as many as 40 per day.
Local
Breaking news and the stories that matter to your neighborhood.
She was eventually diagnosed with CDKL5, a little known genetic disorder. Harper couldn’t walk, talk or even make eye contact. She depended on her parents for everything.
Harper Howard's Journey Through CDKL5
“The first three years of Harper’s life were just a blur … of hospital visits, of treatments and procedures and just trying to keep her alive,” Howard said. “All she was really doing was existing.”
The Howards always knew Harper would die at an early age. Even though experts still know little about her condition, one thing was clear: she didn’t have much time.
So when Harper died in 2016, just shy of her sixth birthday, the Howards donated her brain, tissue and blood to medical research. Harper’s death would not be in vain.
Some of that brain tissue traveled from the family’s home in Texas to Philadelphia where it is now being studied by Dr. Frances Jensen, chair of neurology at Penn Medicine. She hopes to pinpoint what causes CDKL5 and what treatments, if any, can be used to pacify the seizures.
The exact number of people afflicted with CDKL5 is unknown, but experts estimate there could be several hundred patients in the U.S. It is considered an orphan disease because it has largely gone unstudied.
Like others with the condition, Harper’s life was carefully monitored but not necessarily improved by traditional medicine.
Then, in 2013, the Howards stumbled on Real Scientific Hemp Oil (RSHO), a cannabis-based treatment without high-inducing properties that was gaining traction with families in Brazil and Mexico. Because RSHO doesn’t contain THC, it was legal but not necessarily well-known in the United States.
Within the first three days of using RSHO, Harper’s seizures subsided and she made eye contact with her parents, Howard said. While she still couldn’t speak, Harper attempted to communicate by making small sounds. Soon, several days would pass without a seizure and her parents noticed that underneath her disability, Harper was actually a very sassy little girl.
“She could participate in what we did,” Howard said.
Epilepsy frequently comes up in the medical marijuana debate. Last year, British company GW Pharmaceutical released findings in clinical trials for a new anticonvulsant, Epidiolex, a liquid form of cannabidiol that contains no THC. It reduced the number of seizures in patients with Lennox-Gastaut and Dravet syndromes, both rare and severe forms of early-onset epilepsy. When combined with traditional treatment, Epidiolex decreased the number of monthly seizures in young patients by up to 42 percent.
Mexico has also started importing the same medication that helped ease Harper’s overactive brain. RHSO is being used to treat at least one little girl with hypoxia in a small rural town in Veracruz. Like the Howards, the parents of Alina Maldonado Montes de Oca tried at least 14 different medications. Each one came with its own set of unbearable side effects, including liver damage and gastritis.
Maldonado’s father petitioned the Mexican government to allow RSHO to cross international lines and, in 2016, won.
Still little is known about why cannabis-based treatment relieves seizures and other symptoms associated with early onset epilepsy. And in the U.S., studying marijuana remains restricted. It cannot be studied without getting permission from local, state and federal governments.
That is starting to change. At Penn Medicine, Dr. Jensen is about to try something she previously hadn't considered as a neuroscientist: administering cannabis to mice.
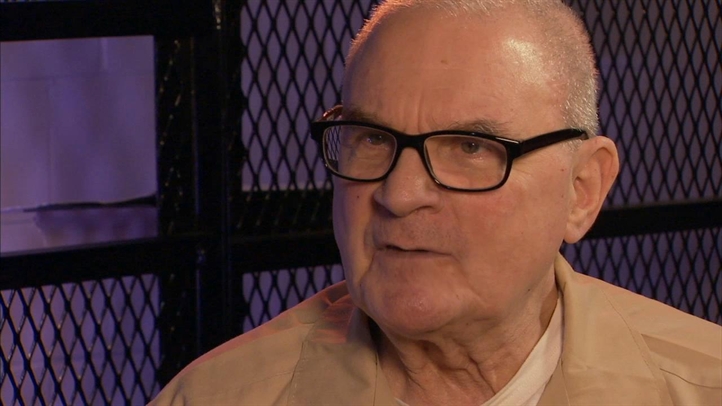
“I wasn’t looking at cannabidiols at all,” she said. “But there is some evidence, from clinical trials, that there are certain subsets of patients that seem to respond, at least partially.”
Since the medicinal pot debate started, countless families have used cannabis to treat everything from cancer to multiple sclerosis. In Pennsylvania, state Sen. Mike Folmer, who co-sponsored the medical marijuana program, admitted to crossing state lines to get cannabis while undergoing chemotherapy for non-Hodgkin lymphoma. His wife also used it to treat chronic pain. These types of stories have propelled research into uncharted territories.
But questions remain:
“How safe are they in the developing brain? Is it safe in normal brains, or is it only safe in brains that have really bad seizures and it’s a way to get the seizures to come down? These are all questions that need answers,” Dr. Jensen said.
To answer some of these mysteries, Dr. Jensen and her team are using Harper’s brain and an army of lab mice.
To date, Dr. Jensen has made an annoying discovery: the brain of someone with CDKL5 doesn’t look all that different from a normal brain on the surface. So they have to keep digging.
“We keep a brain slice alive for many hours, and we can be recording from the cells talking to each other,” she said. “We can see them have mini-seizures, or hyper excitability, and we can then try out drugs to see if the drugs block that abnormal activity.”
For Penny Howard, her daughter's generosity in the after life helps Penny appreciate their time together even more.
“For the longest time I couldn’t say Harper’s name without crying,” Penny Howard said. “I had to learn that it’s okay to talk through the tears and talk about her. That’s the first place to start.”